Optimising Healthcare
When Medical Treatment Doesn’t Make Things Better
by Dr Catriona Nguyen-Robertson MRSV
Healthcare is costly and contributes to 7% of Australia’s carbon footprint1. Is it always worth that cost?
While medical care undoubtedly provides many benefits to many people, sometimes treatments can be ineffective and sometimes even downright harmful.
As a clinician, Professor Rachelle Buchbinder constantly wanted to determine what was best for her patients. How could she best diagnose and treat them? This mentality taught her to ask questions and investigate where scientific evidence behind any clinical practice came from. She did not take anything for granted.
Rachelle has spent decades combining clinical practice with research, investigating ways to reduce waste in the health care system, and identifying more efficient and effective diagnosis and treatment methods. She was awarded the 2022 RSV Medal for Excellence in Scientific Research for her research relating to the treatment of musculoskeletal conditions, as well as work to improve communication with patients and general health literacy.
It’s all about communication: improving public health by improving messaging
Almost everyone experiences low back pain at some point in their lives. In the decade leading up to 1997, it was proving quite debilitating in the workforce: workers’ compensation costs for back-pain claims tripled and rates of back pain were rising. The Victorian WorkCover Authority launched a media campaign that ran from 1997-1999 in response: “Back Pain: Don’t Take It Lying Down”.
The main goal of the campaign was to encourage people with low back pain to take charge of their own recovery. A key message was that they should continue with their usual routines rather than resting for prolonged periods. There is a lot people can do to help themselves recover, and therefore the idea was to avoid people seeking unnecessary medical treatment. The message was widespread, especially at the beginning: it was on television, on the radio and plastered on billboards. But how successful was the campaign?
Rachelle was tasked with evaluating its effectiveness2. She found that there had been a great shift in attitudes among doctors and the general population around back pain beliefs following the campaign. The number of WorkCover claims fell by over 3,000, and there were reductions in the amount of time taken off work and medical costs associated with back pain. Although the campaign had been successful at the time, 20 years later the over-medicalisation of back pain remains a problem.
To combat this, Rachelle led an international team of authors to publish a series of papers3 in The Lancet in 2018 calling for urgent global action to address low-value care for low back pain. The team worked with advocacy and policy consultants to raise public awareness of the issue, resulting in 594 media stories being published across 41 countries. In addition, they devised a Twitter campaign, #LowBackPain, which was seen by almost 15 million people. Importantly, the scientific accuracy of media coverage of low back pain was excellent during the campaign itself, however, it did not translate to long-term accuracy. The media regressed back to containing stories that sell unvalidated products and inaccurate messages.
Rachelle therefore advocates for media advocacy combined with changes in national policies that restrict the marketing of inaccurate messages for back pain. By influencing large numbers of people simultaneously, well-designed health messages have the potential to encourage change over time for the better.
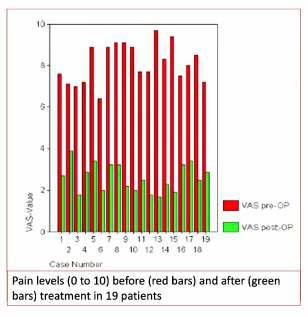
If the average pain reported after treatment (green) dropped compared to before treatment (red), would you believe the procedure works?
Rachelle highlighted that the placebo effect had not been taken into account, and yet this is the only data that supported the use of this treatment in clinics.
Fact or fiction: looking into the true benefits of treatments
Only one in 20 medical treatments have high-quality evidence to support their claimed benefits4. It is particularly worrying that the harms of healthcare interventions are not always quantified. For a doctor or patient to be properly informed when deciding whether to use a treatment, they need to know whether the benefits outweigh the harms. If the harms have been inadequately measured, an “informed choice” is not possible.
The mind is a powerful thing. The placebo effect – the idea that your brain can convince your body that a fake treatment is working – has been around for millenia. But medicine should not simply rely on this. The fairest way to test a treatment is to subject it to a randomised placebo-controlled trial: one group of people receive the active treatment while another receives a “dummy”, and no one knows who received which until the end. This way, any difference in outcome can be attributed to the treatment itself.
Rachelle investigated a common treatment for vertebral fractures caused by osteoporosis. One of the go-to treatments is vertebroplasty, an injection of cement into the fracture to seal it. However, the data supporting its presumed benefits did not stem from a randomised controlled trial. When Rachelle looked into it, she found that it was ineffective – no better than the placebo. Furthermore, sometimes the treatment could be harmful if the cement became dislodged and ended up in a lung or the heart. With a vertebral fracture occurring every 22 seconds worldwide in people over age 505, Rachelle openly voiced her concern to prevent potential harm to patients for whom this treatment was being recommended.
But Rachelle’s finding was not popular among the community for whom vertebroplasty was a lucrative business. She quickly learned that publishing unpopular results could lead to personal attacks. Some clinicians retaliated by claiming that her study was “fake news”, a sham.

It can be hard to investigate accepted treatments and speak against loud voices. But despite pushback, Rachelle forged ahead, and has since built a list of other treatments that we now know have no or limited true benefits. We therefore need to be sceptical of unproven treatments and question where conclusions around their effectiveness come from. Rachelle thus encourages doctors to question data, and patients to ask questions of their doctors and do their own research (e.g. reading lay summaries in the Cochrane Library).
From low back pain to optimising the entire healthcare system
Unnecessary overtreatment costs Australia $30 billion. Furthermore, we could save more than 8,000 kilotons of carbon emissions by scrapping low value care that does not provide any benefit. Most developed countries now spend so much money, and waste so many resources, that healthcare itself has become one of the leading dangers for public health. Only 60% of diagnostics and treatments are effective, while 30% is of no or little value and 10% can be harmful.
Medical professionals may request diagnostic tests and recommend treatments that are unnecessary. Rachelle gave the example of ultrasound-guided injections: while they do have benefits, sometimes a simple injection into the arm would suffice. She worked with clinicians at the Hospital Israelita Albert Einstein in Brazil to establish a consultancy clinic within the hospital to provide a second opinion to patients with degenerative spinal conditions. In doing so, the team found a large discrepancy between the first and second opinions regarding diagnosis and need for spinal surgery. Many patients did not proceed with surgery and had the same outcomes – without the trauma of an invasive procedure.
Doctors want to believe that they are helping their patients. And we want to believe that they are. But sometimes they can overestimate the benefits of certain treatments and underestimate the risks. Not only does this problem in the healthcare system fail to provide benefit and sometimes causes harm, it also diverts scarce resources away from those that need them most. Rachelle is therefore dedicated to optimising healthcare and ensuring that new evidence is translated into practice as soon as it emerges.
References
- Malik, A., et al. (2018). The carbon footprint of Australian health care. The Lancet Planetary Health, 2(1), e27–e35. https://doi.org/10.1016/s2542-5196(17)30180-8
- Buchbinder, R. (2008), Self-management education en masse: effectiveness of the Back Pain: Don’t Take It Lying Down mass media campaign. Medical Journal of Australia, 189: S29-S32. https://doi.org/10.5694/j.1326-5377.2008.tb02207.x
- The Lancet: Low Back Pain series. From https://www.thelancet.com/series/low-back-pain
- Howick, J., et al. (2022). Most healthcare interventions tested in Cochrane Reviews are not effective according to high quality evidence: a systematic review and meta-analysis. Journal of Clinical Epidemiology, 148, 160-169. https://doi.org/10.1016/j.jclinepi.2022.04.017
- Johnell, O., & Kanis, J. A. (2006). An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporosis international, 17(12), 1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Video Presentation
Watch Professor Rachelle Buchbinder‘s presentation to the Royal Society of Victoria on 8 December, 2022 titled “Optimising Healthcare for People with Musculoskeletal Conditions.”