From Ink to Organ: The Power of 3D Bioprinting
By Haireya Abudureheman,
Bachelor of Biomedicine student, The University of Melbourne
Imagine you could create any living structure with just a click. What would you create?
Thanks to advancements in technology, this isn’t just imagination or science fiction – it’s the reality of bioprinting.
Since 3D printing has become cheaper and more popular, it has been utilised across many fields: from small-scale customised jewellery to large-scale car and house manufacturing. Recently, it has started to attract biomedical researchers as they develop innovative solutions to address critical challenges in modern medicine.
Organic challenges
A chronic shortage of organ donors leaves patients on long transplant waiting lists, often with life-threatening consequences. Currently, there are around 1,800 Australians on the waitlist for an organ transplant, and an additional 14,000 on dialysis who would greatly benefit from a kidney transplant.1 However, very few people die in a way that allows for their organs to be used, and the list of patients needing transplants is always longer.
For those patients who do receive a donated organ, they face a different challenge for the rest of their lives: tissue rejection. The immune system has elaborate and effective mechanisms to protect the host against anything it considers to be “non-self”. Transplanted tissue often falls under this category, meaning that it is attacked by the recipient’s immune system. Without a life-long regimen of immunosuppressive drugs to protect it, the transplanted organ can be destroyed.
Making “non-self” look more like “self”
By creating functional, lab-grown organs tailored to individual patients, bioprinting not only reduces reliance on donors but also mitigates the risks of rejection, so that transplant recipients need not remain on immunosuppressive medications for the rest of their lives.
Another major application of bioprinting is testing patient samples to develop personalised treatments, as bioprinted organs can mimic the intricate structure and function of human tissues far better than traditional models. This can lead to safer and more effective therapies, particularly for complex conditions.
Successfully bioprinting organs is therefore a very appealing option.
What is 3D bioprinting?
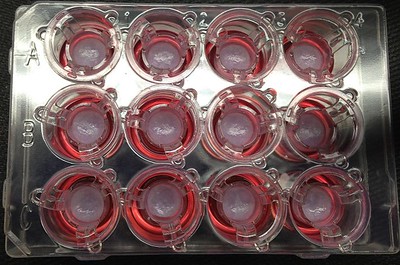
3D bioprinting uses the same layer-by-layer printing technique as traditional 3D printing to construct three-dimensional structures from digital designs.2 Instead of plastic, it uses ‘bio-ink’, made from living cells and various chemicals that support their survival, such as growth factors. The living cells can be sourced from either a donor or the patient themselves, allowing researchers to create patient-specific body parts like organs and other tissues.
There are several 3D bioprinting methods, but in essence, the bio-ink is loaded into a printing chamber and extruded through a moving nozzle to lay down cells in the correct formation. As each layer is added individually, the cells form tissue that (ideally) has all of the structural intricacies of the original organ, including empty channels for blood vessels.
The applications of 3D bioprinting
The use of 3D bioprinting is already well-established in technologies such as lab-grown organs and organ-on-a-chip devices for research. The latter involves labyrinths of tiny channels and tissues in which researchers experiment on the micro- and nano-metre scale. They can be personalised with patient samples, enabling experimentation with a patient’s cells and tissues outside the body. This innovative technology allows them to create patient-specific customised body parts to maximise treatment outcomes. Moreover, bioprinted tissues can also be used for drug testing to reduce the current reliance on animal testing.
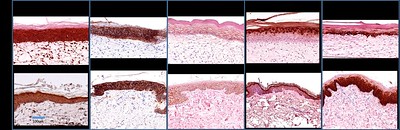
Researchers now aim to use 3D bioprinting technology to print organs for transplantation. Already, there has been successful use of 3D bioprinting technology to create a bladder (1999), prosthetic leg (2008), jaw (2012), and skin (2018).3 One patient who received a 3D bioprinted bladder transplant reported that their bioprinted organ is still fully functional decades after their transplant.4

Two years ago, scientists performed the first transplantation of a 3D bioprinted ear. The 20-year-old patient was born with a small and misshapen right ear, with no externally connected ear canal. The bioprinted ear was grown in stages, starting with cells responsible for producing cartilage, and combining them with a collagen-based bio-ink. The bioprinted ear was then transplanted, successfully reconstructing the patient’s external ear.5
As research continues to progress, the use of 3D bioprinting is extending to more and more organs and tissues.
Challenges of 3D bioprinting
Despite positive advancements in this technology, it is still difficult to build complex organs like heart, lungs or liver. Additionally, ensuring sufficient blood and oxygen supply to a full-sized bioprinted organ presents a significant challenge.
Maintaining the health of the cells in the bio-ink both before and after printing is equally challenging, since the cells can be physically destroyed if the nozzle of the tube is too small, or the printing pressure is too high. Careful consideration of a range of factors is therefore critical for successful bioprinting of any kind.
The future is bright
3D bioprinting is a revolutionary technology that provides us hope for addressing one of the trickiest problems in the medical field. Researchers aim to develop full-sized, complex organs in the future, as well as enhanced personalisation of treatments and transplants.6
Hopefully technologies like 3D bioprinting can help to ensure that anyone in need of an organ transplant isn’t confined to the bottom of a long wait list.
References:
- Statistics in Australia. (2023). DonateLife. www.donatelife.gov.au/all-about-donation/statistics-in-australia#Latest-stats
- Lewis, J. (2019, February 22). 3D Bioprinting of Living Tissues. Wyss Institute. wyss.harvard.edu/technology/3d-bioprinting/
- Price, D. (2015, March 19). CloudTweaks | The History Of 3D Printing – From Kidneys To Cars. CloudTweaks. cloudtweaks.com/2015/03/3d-printing-history-organs/
- Padraig Belton. (2018, September 10). “A new bladder made from my cells gave me my life back.” BBC News. www.bbc.com/news/business-45470799
- Ravisetti, M. (2022, June 3). In a World First, Scientists Transplant 3D-Printed “Living Ear” Onto Patient. CNET. www.cnet.com/science/biology/doctors-3d-print-living-ear-and-transplant-into-patient/
- Gaget, L. (2018, February 21). 3D bioprinting: What can we achieve today? 3D Printing Blog | Sculpteo. www.sculpteo.com/blog/2018/02/21/3d-bioprinting-what-can-we-achieve-today-with-a-3d-bioprinter/