A Sweet Solution To The Sugar Problem
Science Victoria Edition

By Dr Catriona Nguyen-Robertson MRSV
Senior Editor, Science Victoria
Prior to the mid-20th century, a type 1 diabetes diagnosis was a death sentence. Your only option was to starve yourself of carbohydrates to limit the amount of sugar in your blood, which bought you a few extra years at most. Some patients even died of starvation after being prescribed as few as 450 calories a day – just over a quarter of the recommended daily caloric intake.1

Although we still have no cure for diabetes, advancements in insulin therapy have meant that the lives of diabetics aren’t cut tragically short. The discovery of insulin and its role in treating diabetes, and the development of ways to provide patients with regular doses of it were decades in the making.
Insulin and its discovery
Insulin is a hormone that controls blood sugar (glucose) levels – if the level is too high, insulin signals for cells throughout your body to take up glucose and for your liver cells to convert glucose to glycogen, a type of fat, for storage.
In 1889, two German researchers, Oskar Minkowski and Joseph von Mering, found that when the pancreas gland was removed from dogs, the dogs developed symptoms of diabetes.2 This led to the idea that the pancreas was the site where “pancreatic substances” (what we now know as insulin) were produced, which was then narrowed down to specific clusters of specialised cells.
In 1910, Sir Edward Albert Sharpey-Shafer suggested that it was only one chemical that was missing from the pancreas in people with diabetes.3 This chemical controlled blood sugar, which he called insulin, from the Latin insula (“island”).3
We now understand that type 1 diabetes is an autoimmune condition in which a person’s own immune system attacks and destroys the insulin-producing cells. Specialised immune cells – that usually do not enter the pancreas – gain access, and once they have destroyed enough of the insulin-producing cells, the pancreas no longer produces insulin.
Understanding the cause of the disease meant that researchers could now work out a way to treat the condition.
A lifesaving, murky concoction
Attempts were made to extract insulin from ground-up pancreas cells, but they all proved unsuccessful. The challenge was to find a way to extract insulin from the pancreas without it being destroyed in the process.
In 1921, Canadian surgeon Frederick Banting figured out how to extract insulin from a dog’s pancreas and keep it intact. Banting had read an article suggesting that the insulin-producing cells are specifically slower to deteriorate than other pancreatic tissue, meaning that he could possibly break down the pancreas in a way that would leave them intact.
As Banting wasn’t a scientist by training, he couldn’t test his theory alone, and visited John Macleod, a professor at the University of Toronto.
Macleod was sceptical that a research novice would succeed when others had failed, but he saw the value in Banting’s surgical skills to be able to test pancreas grafts and transplantation (an idea for treatment that had been floating around at the time).4 He offered Banting dogs, lab space for experiments, and a research assistant, Charles Best.
While many of their initial experiments failed, the three worked together to produce an extract.5,6 They tied off the pancreatic duct of dogs to cause the pancreatic tissue to die – and extracted insulin from what was left behind to create a “thick, brown muck”.5,6

With this murky concoction, Banting and Best kept another dog with severe diabetes (having completely removed its pancreas) alive for 70 days.5,6 Thanks to their extract, they saw regular drops in blood sugar levels, with the dog only dying when there was no more of the extract available. 5,6
Having seen success in dogs, the researchers, along with biochemist James Collip worked towards a more refined form of insulin, this time from the pancreases of cattle.
The very next year, in January 1922, a 14-year-old boy dying from type 1 diabetes received an insulin injection.7 While the first try was unsuccessful, a second shot dropped his dangerously high blood sugar levels to near-normal levels.7 He was the first person to be treated, and many have followed since.
Word of insulin’s success spread, and in recognition of their life-saving discovery, Banting and Macleod were jointly awarded the 1923 Nobel Prize in Physiology or Medicine. Banting split his half of the Prize money with Best, and Macleod did the same with Collip.
Insulin on demand
With 830 million people worldwide currently living with diabetes,8 and each of them requiring regular injections of insulin to keep their blood sugar in check, insulin needed to be produced on a large scale.
The medical company Eli Lilly started large-scale production of insulin isolated from cattle and pigs. Cow and pig insulin were used for many years to treat diabetes and saved millions of lives, but it wasn’t perfect, as it caused allergic reactions in many patients.9
Instead, Eli Lilly turned to biotechnology. Not only would this mean that they could synthetically produce human insulin specifically, it also meant that production could be scaled up even further.
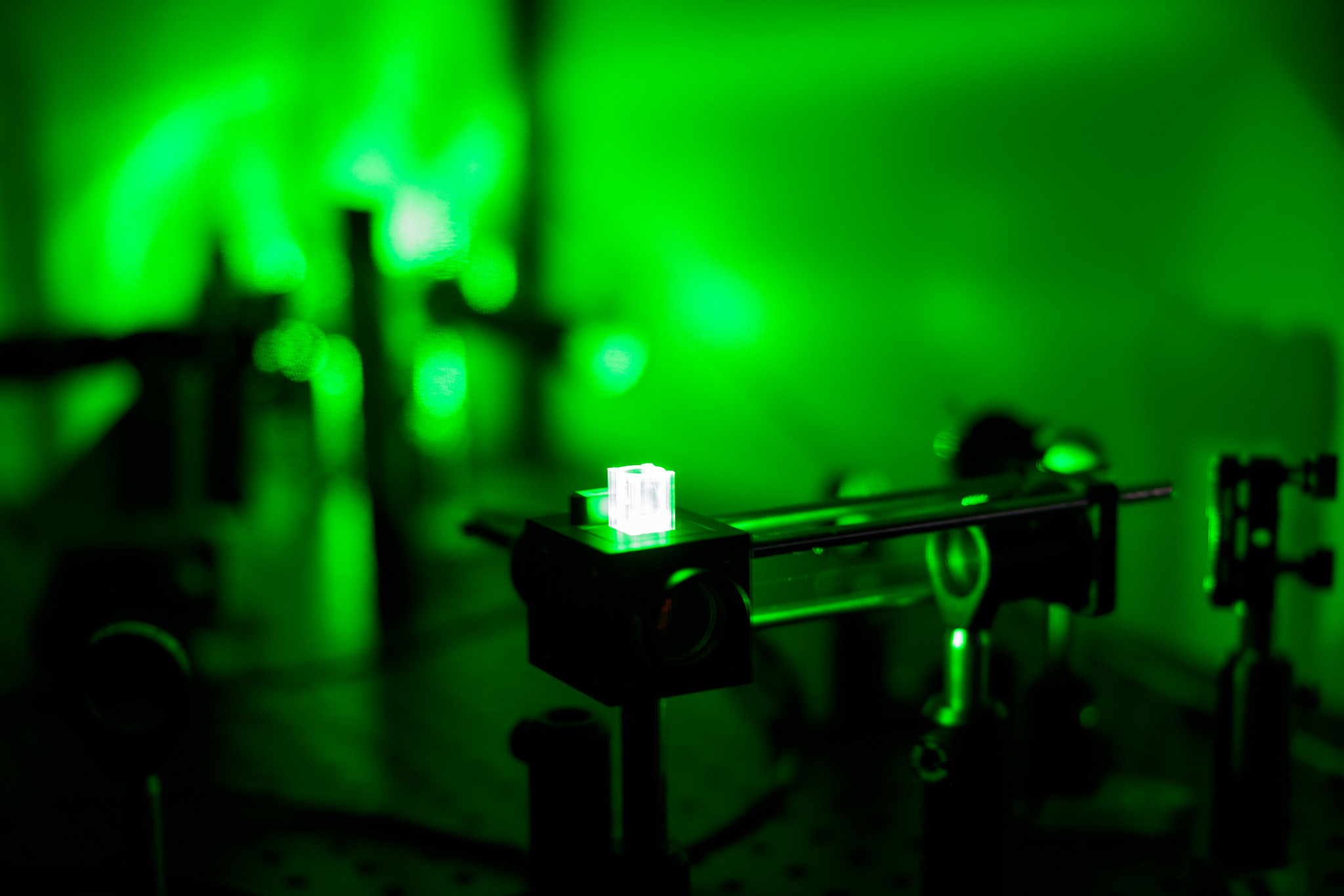
The first synthetic “human” insulin was produced in 1978 using genetically engineered E. coli bacteria. Scientists cut and paste the human insulin gene into a loop of bacterial DNA, which allows for the gene to be introduced into the bacteria. Bacteria that take up the DNA read the instructions from the inserted gene to make the insulin protein.
Insulin now comes in many forms, from regular human insulin identical to what the body produces on its own, to ultra-rapid and ultra-long-acting insulins. By tweaking the genetic instructions provided to bacteria, they can make different forms of insulin 24/7.
Who “owns” insulin?

If biotechnology means that insulin is incredibly cheap to produce, and it’s the only thing that keeps type 1 diabetics alive, who should be profiting off it?
In the US, some diabetics struggle to purchase insulin and try to stretch out their doses to detrimental consequences. They simply cannot afford to live. Thankfully, in Australia, insulin is much more affordable.
Ironically, Banting, Collip, and Best were awarded a patent for insulin and sold it to the University of Toronto for a dollar each. At the time, Banting said, “Insulin does not belong to me, it belongs to the world.”10 He wanted it to be accessible to everyone who needed it.
As biotechnology increasingly solves more of our public health challenges (as well as agricultural and environmental challenges), we need to carefully consider how it is being used and ensure that everyone benefits. Synthetic insulin produced by bacteria in large vats may not be a cure for diabetes, but it is literally a lifesaver.
References:
- World Health Organization. (2020, April 29). Healthy Diet. https://www.who.int/news-room/fact-sheets/detail/healthy-diet
- Kyle, R. A., et al. (2015). Oscar (Oskar) Minkowski: Discovery of the Pancreatic Origin of Diabetes. Mayo Clinic Proceedings, 90(2), e17–e18. https://doi.org/10.1016/j.mayocp.2014.06.026
- Sharpey-Schaffer E. A. (1916). The Endocrine Organs. London: Longmans, Green and Co.
- Bliss, M. (1993). The History of Insulin. Diabetes Care, 16(Supplement_3), 4–7. https://doi.org/10.2337/diacare.16.3.4
- Hegele, R. A., & Maltman, G. M. (2020). Insulin’s centenary: the birth of an idea. The Lancet Diabetes & Endocrinology, 8(12), 971–977. https://doi.org/10.1016/s2213-8587(20)30337-5
- Quianzon, C. C., & Cheikh, I. (2012). History of insulin. Journal of Community Hospital Internal Medicine Perspectives, 2(2), 18701. https://doi.org/10.3402/jchimp.v2i2.18701
- Vecchio, I., et al. (2018). The Discovery of Insulin: an Important Milestone in the History of Medicine. Frontiers in Endocrinology, 9(613). National Library of Medicine. https://doi.org/10.3389/fendo.2018.00613
- World Health Organization. (2024, November 14). Diabetes. https://www.who.int/news-room/fact-sheets/detail/diabetes
- Schernthaner, G. (1993). Immunogenicity and allergenic potential of animal and human insulins. Diabetes Care, 16 Suppl 3, 155–165. https://doi.org/10.2337/diacare.16.3.155
- Lewis, G. F., & Brubaker, P. L. (2021). The discovery of insulin revisited: lessons for the modern era. The Journal of Clinical Investigation, 131(1). https://doi.org/10.1172/JCI142239
Discover how you can join the society
Join The Royal Society of Victoria. From expert panels to unique events, we're your go-to for scientific engagement. Let's create something amazing.